Your questions answered about keratoconus treatments
Learn how corneal crosslinking can stabilise your corneal health, slow keratoconus progression, and enhance your vision and daily life
Take control of your eye health in 3 simple steps
Caring for your eyes doesn’t have to be complicated. Whether it’s retinal care, blepharoplasty, or glaucoma management, here’s how to begin your journey to healthier, clearer vision


Step 1: GET IN TOUCH
Reach out to our team to book a comprehensive eye assessment. Call us at +387 51 439-591 or contact us online to schedule a time that suits you. This is your first step towards better eye health.


Step 2: WE’LL MEET
At your appointment, we’ll conduct a detailed examination of your eye health, assess your specific concerns, and develop a personalised treatment plan tailored to your needs


Step 3: ENJOY FREEDOM
With expert care and tailored treatments, you can enjoy improved vision and peace of mind. We’re here to support you every step of the way, helping you protect and enhance your eye health for the future
Join thousands who have achieved freedom from glasses and contacts
Learn how they overcame their dependence, and find out how you can, too
We have replaced the images of the actual patients who provided these testimonials to protect their privacy
Academic resources on keratoconus
Expand your knowledge about keratoconus. (These links will take you away from our website.)

Hi i'm Dr. Bojan Kozomara
With over 20 years of experience and a PhD in Ophthalmology, I am proud to be a leading expert in eye health.
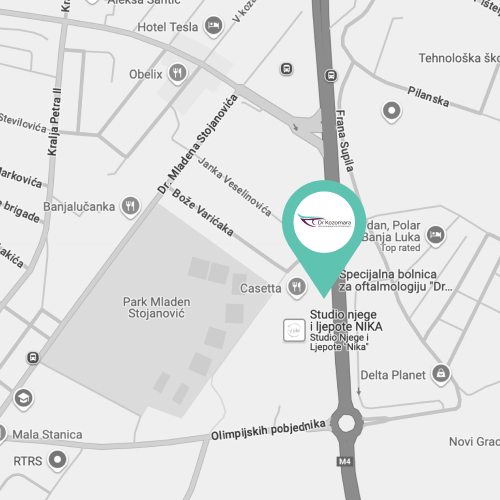
As the Director of the Special Ophthalmology Hospital "Dr. Kozomara," I have performed numerous successful surgeries, specialising in vitreoretinal and phacoemulsification procedures.
My commitment to personalised care and deep expertise allow me to provide trusted, high-quality treatment.
My greatest reward is seeing my patients thrive with improved vision.
Dr Kozomara