Experience the freedom of clear vision
See how LASIK transforms not only your eyesight but also your confidence, comfort, and daily life, bringing a newfound sense of freedom
Discover the freedom of clear vision without glasses
After LASIK, you’ll no longer deal with the hassle of wearing glasses. Say goodbye to fogging, slipping, and discomfort during activities like workouts, yoga, or outdoor sports. Enjoy 20/20 vision without the inconvenience, giving you the freedom to fully enjoy your active lifestyle without limits.
Unlock a new sense of confidence
Without glasses, you’ll feel more confident in everything you do. Whether it’s participating in activities or attending social events, you’ll embrace your new look and enjoy the peace of mind that comes with clear vision and independence.
Make the most of every day
Imagine starting your day by diving into your tasks without the hassle of glasses. Whether you're working, exercising, or meeting friends for lunch, you move through each activity with ease and confidence. Every moment feels lighter, allowing you to fully enjoy your day with a sense of freedom and joy.
Embrace the new you
Your friends and family will notice the positive change in you. They’ll see your confidence and freedom shine through as you live life without glasses. Your energy and happiness will inspire others, and your new look will reflect your vibrant personality, making you feel more approachable and lively.
Experience the freedom of clear vision
See how LASIK transforms not only your eyesight but also your confidence, comfort, and daily life, bringing a newfound sense of freedom

Unlock a new sense of confidence
Without glasses, you’ll feel more confident in everything you do. Whether it’s participating in activities or attending social events, you’ll embrace your new look and enjoy the peace of mind that comes with clear vision and independence.

Make the most of every day
Imagine starting your day by diving into your tasks without the hassle of glasses. Whether you're working, exercising, or meeting friends for lunch, you move through each activity with ease and confidence. Every moment feels lighter, allowing you to fully enjoy your day with a sense of freedom and joy.
3 Easy steps to clear vision without glasses or contacts
Laser eye surgery doesn’t have to be difficult. We’ve simplified the process to make your journey to glasses-free vision smooth and stress-free


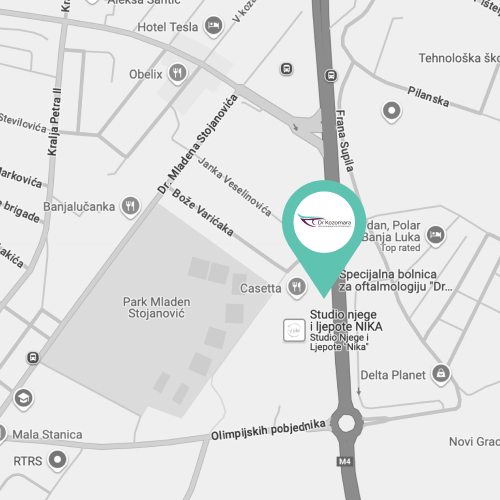
Step 1: Reach out
Ready to experience life without glasses or contacts? Your first step is to get in touch with us. Call our friendly team at +387 51 439 591, or use our convenient online calendar to book an appointment.


Step 2: We'll meet
During your appointment, we’ll assess your eyes, talk about your lifestyle, and answer any questions you have. You’ll receive a personalised recommendation for the best laser vision correction option for you, ensuring you feel confident about your decision.


Step 3: Enjoy freedom
After your laser treatment, you’ll enjoy the freedom of living without glasses or contacts. Many patients are amazed by how quickly their vision improves and how much easier daily activities become. Say goodbye to glasses and contacts, and hello to a brighter, clearer future!
All you need to know about LASIK
Discover how LASIK can improve your eyesight, eliminate the need for glasses or contacts, and enhance your daily life
Are glasses and contacts holding you back?
If so, it's time to take control of your vision and discover the life-changing benefits of laser eye surgery

Tired of constantly dealing with glasses?
You depend on glasses for everything—reading, working, driving. They’re a necessary but annoying part of your routine. Now, imagine living without needing to worry about lenses or frames ever again.
With laser eye surgery, you can restore your vision, boost your confidence, and enjoy the freedom of living without glasses holding you back.

Feeling limited by your look?
If glasses make you feel self-conscious about your appearance or limit your style, imagine the confidence you’ll feel being glasses-free. You’ll have a clearer, more natural look that reflects how you want to see yourself.

Frustrated by how glasses get in the way of your daily life?
In your busy life, glasses are constantly fogging up, smudging, or needing to be taken on and off. From work to social events, they’re a hassle. Picture your life with clear vision—free from these everyday annoyances, so you can focus on what really matters.
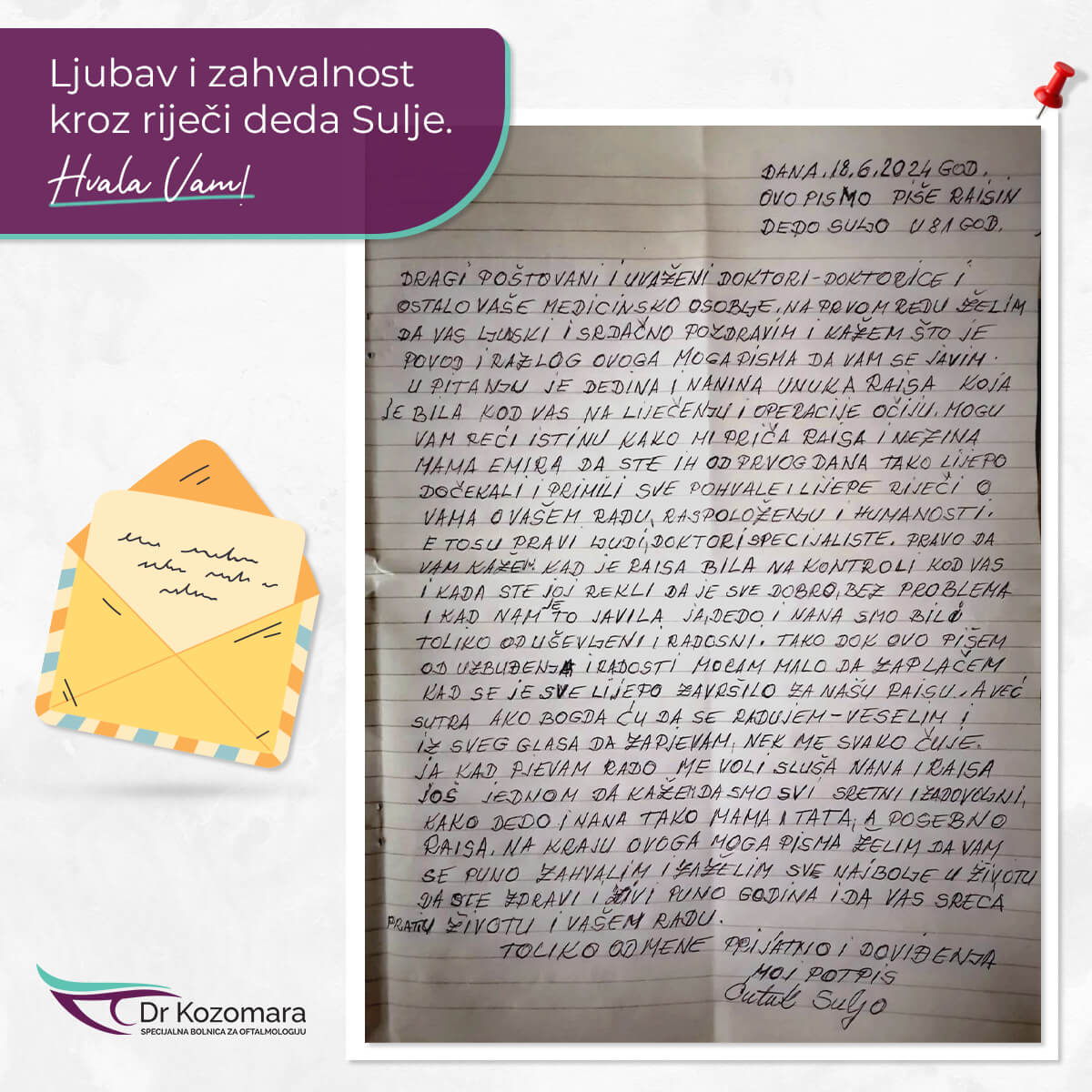
Join thousands who have achieved freedom from glasses and contacts
Learn how they overcame their dependence, and find out how you can, too
We have replaced the images of the actual patients who provided these testimonials to protect their privacy
FAQs and information about vision correction
Everything you need to know about our practice and procedures
Academic resources on LASIK
Expand your knowledge about LASIK. (These links will take you away from our website.)

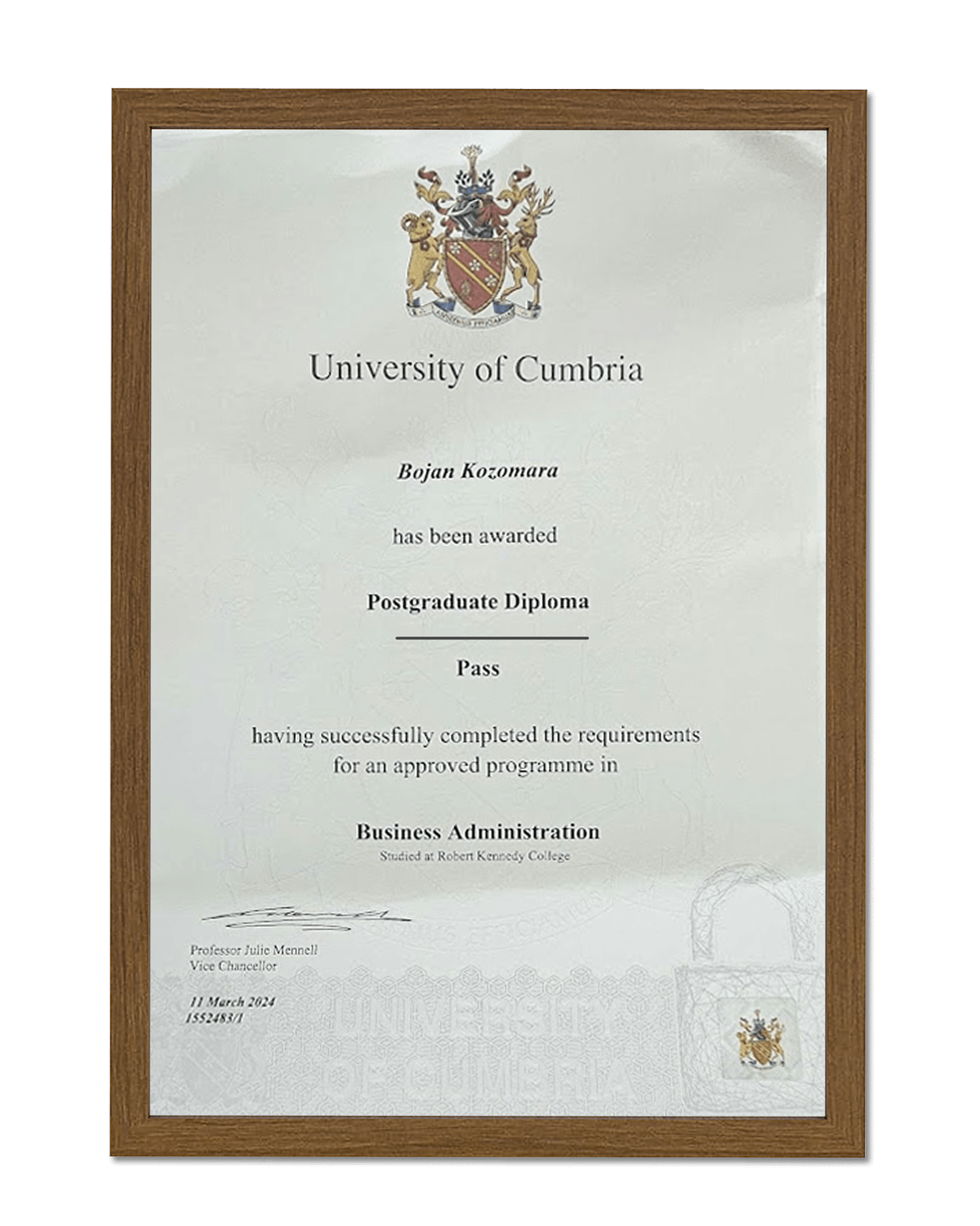
Hi i'm Dr. Bojan Kozomara
With over 20 years of experience and a PhD in Ophthalmology, I am proud to be a leading expert in eye health.
As the Director of the Special Ophthalmology Hospital "Dr. Kozomara," I have performed numerous successful surgeries, specialising in vitreoretinal and phacoemulsification procedures.
My commitment to personalised care and deep expertise allow me to provide trusted, high-quality treatment.
My greatest reward is seeing my patients thrive with improved vision.
Dr Kozomara